Ebola case fatality rate is between 40% to 90%
“The illness has a case fatality rate of between 40% to 90% (depending on the virus species) with SUDV having a case fatality rate of approximately 50% seen in previous outbreaks.”
“If the patient presents to primary care and initial clinical assessment… indicates [Ebola], they should be isolated immediately in an empty room.”
The UK has issued new guidance for GP’s on how to deal with suspected Ebola patients that walk into their surgeries.
Ebolavirus disease presents with a wide range of symptoms, with an incubation period of between 2 to 21 days post-exposure (average 4 to 10 days). The onset of symptoms can be sudden, with fever, malaise, myalgia, and headaches. These symptoms may progress to include rash, nausea, vomiting, diarrhoea and abdominal pain. Internal and/or external bleeding may occur but will not be present in all cases, nor early in illness, and this should not be used as the sole indicator for suspicion of EVD.
There is no definitive treatment regimen for EVD, and clinical interventions are mainly supportive. The illness has a case fatality rate of between 40% to 90% (depending on the virus species) with SUDV having a case fatality rate of approximately 50% seen in previous outbreaks.
There are currently no licensed vaccines for use against SUDV and the current evidence suggests that vaccines against other EVD strains do not provide cross-protection for SUDV. Several trials for SUDV-specific vaccines are ongoing and being led by the World Health Organization (WHO) R&D Blueprint group.
Ebola virus is transmitted from person to person through direct contact with blood, secretions, or other bodily fluids of an infected person. There is no evidence for an airborne route of transmission – transmission via large saliva droplets may be possible but this is an unlikely route of spread.
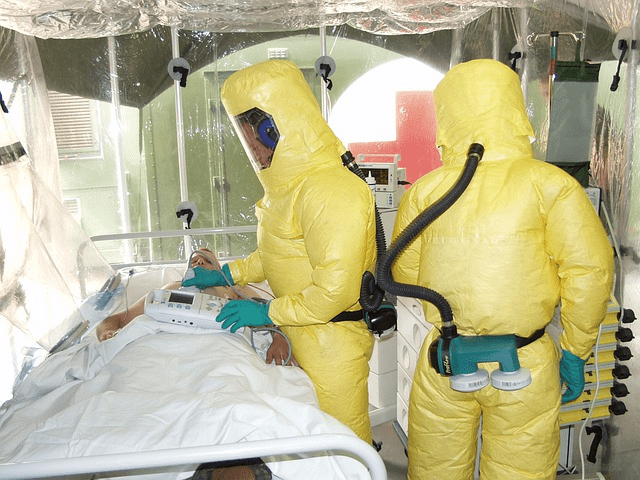
It is important that appropriate PPE and barrier treatment methods are utilised by all healthcare professionals involved in the treatment and management of potential EVD patients (including the deceased) to prevent transmission.
Transmission via environmental contamination is possible so healthcare settings where EVD patients have been treated should be deep cleaned and waste be managed according to national guidelines.
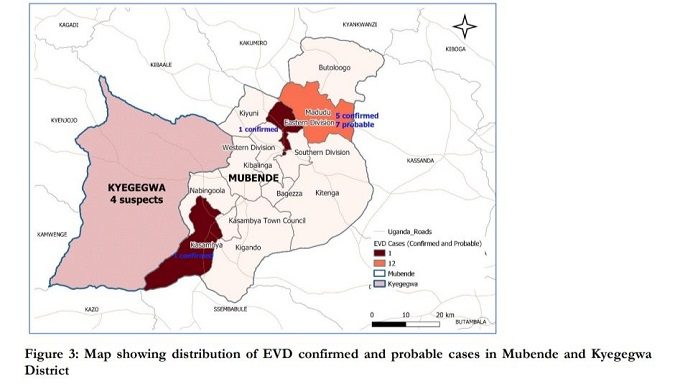
In summary, any febrile patient is eligible for testing if they have become unwell within 21 days of leaving an endemic country and they have visited an area with a current VHF outbreak. During the current outbreak this applies to any patient with a fever who has left Uganda within the past 21 days.
The appropriate PPE is double gloves, fluid repellent disposable gown (or coveralls), full length plastic apron, head cover, fluid repellent footwear, full face shield or goggles, and fluid repellent FFP3 respirator. Safe waste management and decontamination are also required. Full details on PPE and all IPC procedures are provided in the ACDP guidance.
If the patient presents to primary care and initial clinical assessment using the flowchart in the ACDP guidance indicates EVD, they should be isolated immediately in an empty room. The case should be urgently discussed with the local acute infectious disease unit and, if EVD is still suspected, specialist ambulance transfer should be arranged to a dedicated inpatient facility for detailed clinical assessment and treatment.